As we grow older, we occasionally experience memory lapses and “senior moments.” We misplace the car keys or pause to recall a name. Sometimes, we find ourselves in front of the closet, wondering why we came. If these slip-ups increase, then we worry they’re the warning signs of Alzheimer’s.

Just a Senior Moment?
During a real “senior moment,” we realize we forgot something but eventually remember it. Blame it on the fact that human thought processes slow with age.1
While it’s true that memory loss is the best-known symptom of Alzheimer’s2, this form of dementia causes far more than momentary forgetfulness. It significantly disrupts the brain’s ability to both think and reason. The first symptom generally is “unlearning” something you just learned.

Just a Senior Moment?
During a real “senior moment,” we realize we forgot something but eventually remember it. Blame it on the fact that human thought processes slow with age.1
While it’s true that memory loss is the best-known symptom of Alzheimer’s2, this form of dementia causes far more than momentary forgetfulness. It significantly disrupts the brain’s ability to both think and reason. The first symptom generally is “unlearning” something you just learned.
For instance, say you have a long talk with a new neighbor. Then, an hour later, your wife asks what you discussed. If you’ve forgotten everything the two of you said, then that’s more than a senior moment — particularly if you don’t recall meeting the neighbor.
Other warning signs of Alzheimer’s
If you experience the following, it may be time to talk to your doctor.
- Frequently lose track of the date and time of day or of where you are
- Forget you’ve asked a question, then repeat it over and over
- Need extra reminders to keep regular routines
- Struggle with tasks performed in a particular order (e.g., getting dressed, making a sandwich)
Alzheimer’s: It takes two
Memory loss might be a warning sign of Alzheimer’s when it
- Gets in the way of ordinary, everyday life AND
- Is joined by new difficulties with
- Planning, problem-solving or judgment (cognitive skills)
- Communication – especially using the right words (language skills)
- Attention and concentration or
- Understanding what you see (visual perception)
Doctors diagnose dementia if severe difficulties with at least two of the brain’s principal functions interfere with daily life.3
Alzheimer’s also gets worse
When doctors call Alzheimer’s a progressive disease, they mean its symptoms worsen. So, you might suspect Alzheimer’s if
- Aunt Joan grows unusually distant at family gatherings. Quickly losing the thread of group discussions, she’s increasingly agitated — paranoid that people haven’t shared family news with her. Eventually, she finds excuses not to attend or sits quietly in the corner.
- Mom once prided herself on being punctual. Lately, though, she’s showing up late to regular appointments. One day she doesn’t show up at all — then calls hours later, hopelessly lost.
- Dad complains that the bank has been making lots of mistakes lately. While examining his desk, you discover overdraft slips and unpaid bills jammed in a drawer. It also looks as if he stopped balancing his checkbook months ago.
- Grandpa, once a dapper dresser, spends most days in his pajamas. He seems to have lost track of his sleep schedule. You suspect he’s missing his meds and meals, too.
Alzheimer’s also gets worse
When doctors call Alzheimer’s a progressive disease, they mean its symptoms worsen. So, you might suspect Alzheimer’s if
- Aunt Joan grows unusually distant at family gatherings. Quickly losing the thread of group discussions, she’s increasingly agitated — paranoid that people haven’t shared family news with her. Eventually, she finds excuses not to attend or sits quietly in the corner.
- Mom once prided herself on being punctual. Lately, though, she’s showing up late to regular appointments. One day she doesn’t show up at all — then calls hours later, hopelessly lost.
- Dad complains that the bank has been making lots of mistakes lately. While examining his desk, you discover overdraft slips and unpaid bills jammed in a drawer. It also looks as if he stopped balancing his checkbook months ago.
- Grandpa, once a dapper dresser, spends most days in his pajamas. He seems to have lost track of his sleep schedule. You suspect he’s missing his meds and meals, too.
If the warning signs point to Alzheimer’s or another form of dementia . . .
Then call your doctor — the more rapid the onset, the more critical the need to see them.
Why bother if the diagnosis most likely is Alzheimer’s’?
- More than 50 medical conditions cause dementia or memory loss.4 Your doctor should rule out the others.
- Some forms of non-Alzheimer’s dementia can be halted – or reversed – with early diagnosis and treatment.
- Doctors treat the underlying causes of dementia. They address Alzheimer’s differently than thyroid disease or drug reactions.
- Medical treatment may relieve some of your loved one’s most troubling symptoms.
- Trained professionals can show you how to give better, more comforting care.
- Early diagnosis permits a person to make plans and clearly express their wishes.
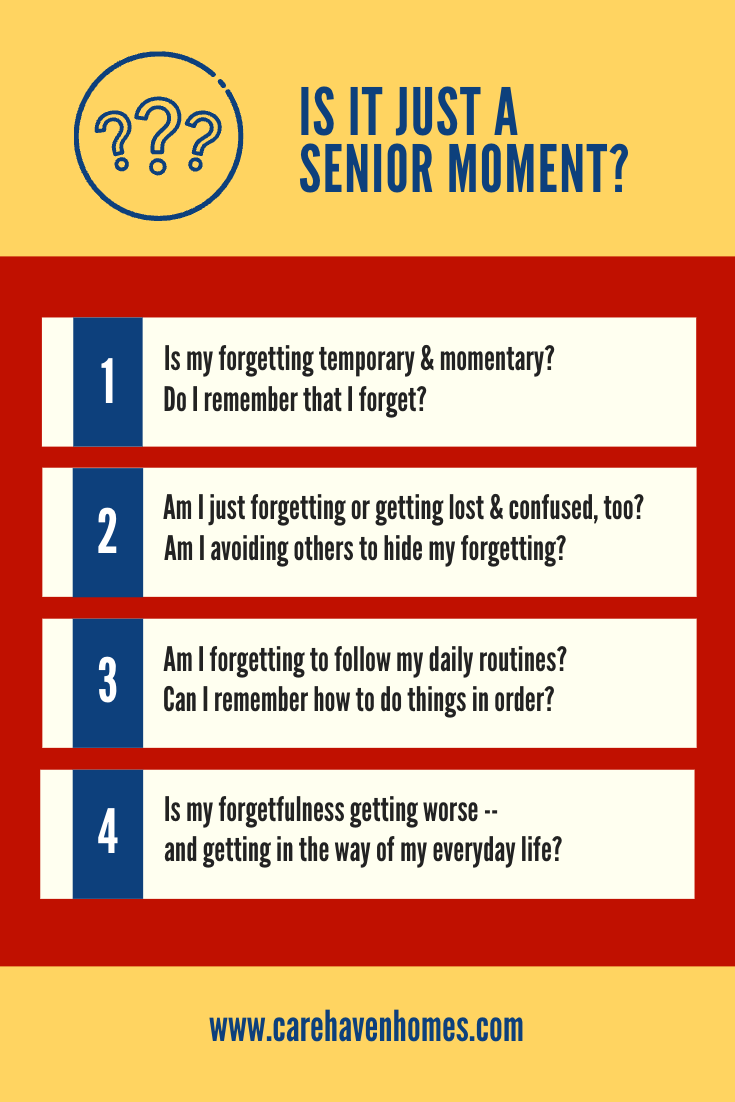
To prepare for your visit, take detailed notes on warning signs that alarm you. The infographic below can help you identify and cope with symptoms. (Be sure to scroll below the graphic for more detailed information.)
1. Alzheimer’s is not just memory loss
Alzheimer’s strikes the wrinkled outer layer of the brain – our “gray matter” – called the cortex. It spreads in a predictable pattern.
First, it strikes areas that control learning and memory. Next, the damage spreads to areas responsible for thinking, planning and problem-solving, or “executive function.” (A telltale warning sign of Alzheimer’s is sudden difficulty handling one’s finances.)
During Alzheimer’s’ middle stages, symptoms further impact
- The ability to talk and understand the spoken word. People with Alzheimer’s sometimes speak a “word salad,” tossing words together in a random, confusing mix.
- The sense of where you are within the environment – or where objects are in relation to each other- is called visuospatial dysgnosia. As a result, someone with Alzheimer’s may find it difficult to
- Copy a drawing
- Find their way home
- Reach for and grasp a glass of water
- Follow a moving object with their eyes without turning their head or
- Fit clothing over body parts while dressing
Struggling to follow and join conversations, some people living with Alzheimer’s seem to change their personalities. As moving about and making good choices grow challenging, most need help with daily activities, too. It’s no longer safe for them to live alone.
Odd symptoms might pop up in Alzheimer’s later stages, again due to changes in the brain. The room seems too hot or cold, and occasionally imaginary strangers visit. You may notice that your loved one struggles to spear meat with a fork, finding it difficult to distinguish between food and the plate. (Try a brightly colored dish for more contrast!)
2. Alzheimer’s can be hard to swallow
In the early stages of Alzheimer’s, symptoms appear at the tip of the tongue. People have trouble finding the right word. Eventually, tasting and swallowing are affected, too.
Everyone’s taste buds dull as we age. Subtle flavors disappear, so food doesn’t taste the same. For that reason, even people who once shunned desserts are likely to develop a sweet tooth.
But those with dementia undergo more dramatic changes. For instance, they may not recognize the food on their plates. Or they might forget how it’s supposed to taste. Add difficulty using silverware and chewing, and it’s no wonder their food preferences change as the disease progresses. As a result, it can be challenging to keep someone with Alzheimer’s engaged in the critical task of eating.
However, the most dangerous warning sign of Alzheimer’s at the dinner table is difficulty swallowing. At first, you might notice drooling, coughing, hoarseness or throat clearing. You also could detect shortness of breath or find that food gets stuck in your loved one’s throat, then comes back up.
Severe swallowing problems could lead to
- Weight loss
- Choking or
- Pneumonia
So, make mealtime safe and enjoyable by taking it easy
- Allow plenty of time – an hour or more – and go slow
- Avoid noise and distractions that make it difficult to focus on eating
- Simplify the table setting
- Serve just one or two foods at a time
- Serve old favorites – but be flexible as food preferences change
- Prepare easy-to-eat meals, opting for finger foods to avoid silverware struggles
- Gently remind your loved one to chew and swallow
- Be sure they sit up straight, with their chin tucked slightly to assist in swallowing
- Be alert to signs of choking
(For more advice about the dinner hour, visit the Alzheimer’s Association’s Caregiver Center.)
3 – The warning signs of Alzheimer’s are not just in your head
Long before forgetfulness strikes, the muscles of a person with Alzheimer’s start to weaken. Scientists aren’t sure how or why. They believe a single degenerative process attacks both cognitive function AND muscle strength.
As a result, people with Alzheimer’s may shuffle or quickly lose their balance. Eventually, they may find it challenging to stand, sit in a chair, hold up their heads or smile.
There are bowel and bladder issues, too. In the beginning, these result primarily from
- Other medical conditions
- Medication side effects
- Mobility issues or physical obstacles that slow the trip to the bathroom
- Difficulty removing clothing
- Confusion about where the toilet is or how to use it
- Distraction – or depression and apathy
- Poor communication skills
- Embarrassment at needing help
Under those circumstances, caregivers use continence management strategies to avoid accidents and toileting problems.
During the very late stages of Alzheimer’s, the brain no longer relays the signals that regulate continence. Disposable garments then become essential.
5 – With Alzheimer’s, live in the now
We grow frustrated by watching our loved ones change. From time to time, we try to prod them back to their old selves.
- “Look at the picture and think hard. You can’t forget your grandson!”
- “I’ve answered that question a million times, Mom. This time, listen more carefully.”
- “I won’t help you make that sandwich. Practice doing it yourself. Use It or Lose It!”
Alzheimer’s is a progressive disease. We won’t slow it with criticism or corrections. We’re better caregivers when we accept circumstances for what they are and focus on supporting our loved ones,
- Protecting them from unnecessary stress, fear or pain
- Preserving meaningful social connections
- Showering them with compassion, patience and kindness
Try your best to
- View challenging behavior as a response to dementia’s symptoms
- Remain calm, refusing to take things personally
- Look past your loved ones’ actions to their feelings
- Keep EVERYTHING simple, quiet and relaxed
- Acknowledge small successes and simple pleasures
- Join your loved one in their current reality – even if today they’re living in the distant past
Most importantly, remind them that they’ll always be a cherished member of your family.
More on the warning signs of Alzheimer’s
Online resources can keep you abreast of current findings and practices. (That includes links in the article above and the sources below.) We highly recommend the National Institute on Aging’s Education and Referral Center for thorough, easy-to-understand information.
Sources
2 “What Is Dementia?” Alzheimer’s Association. Alzheimer’s Association, n.d. Web. March 2020.
3 Ibid.